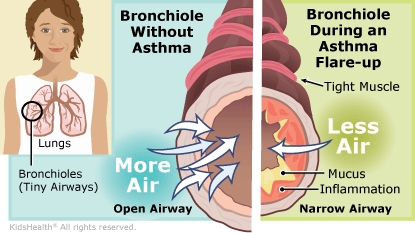
An asthma flare-up (also called an asthma attack or exacerbation) is when asthma symptoms get worse. During an asthma flare-up, the muscles around the airways tighten. The lining of the airways gets inflamed, causing it to swell and fill with mucus. All these changes make it hard to breathe. A child having a flare-up may cough a lot, wheeze, feel chest tightness, or be short of breath.
During your child's stay in the hospital, the health care team gave medicines to help control the symptoms. They checked your child often and were able to increase the time between the doses of medicine. Your child can now be cared for at home.
The health care provider might have given you an asthma action plan or reviewed the plan with you and your child if you already have one. An asthma action plan is a set of instructions that detail how to manage asthma at home. Keeping the plan up to date and following it closely can help a person prevent or treat symptoms and keep their asthma under control. It's important that you and your child understand the asthma action plan, know the signs of a flare-up, and know what to do if a flare-up happens.

As your child gets better from this flare-up:
When your child's breathing is back to normal:

Your child:
Your child has trouble breathing. Signs you might see include:
Call 911 if your child is struggling to breathe, is too out of breath to talk or walk, or turns blue.

What is asthma? Asthma is a condition that causes breathing problems. It is a chronic (ongoing) condition, which means it usually lasts for years, though many kids grow out of it. Asthma can be mild or so severe that it gets in the way of daily activities. But with medicine and the right care plan, asthma symptoms can be managed so that kids can do just about anything they want to do.
What are common asthma triggers? Triggers can bring on asthma symptoms, but they don't cause asthma. Triggers are different for each person with asthma, but common ones include:
How do asthma medicines work? Asthma medicines generally work in two ways:
Some children will get both types of medicines from one inhaler device. They might need to use this "combination" inhaler every day, with added doses from it when they have symptoms. Some older kids with mild asthma might use a combination inhaler only for quick relief when they have symptoms, or before they exercise. Your health care team will help you figure out which inhaler is best for your child, and how and when to use it.
Are all asthma medicines breathed in, or can some be taken by mouth? Some medicines that ease inflammation can also be taken by mouth. For example, health care providers may prescribe oral steroids for inflammation during a flare-up, usually for 5–7 days.